
Frequently Asked Questions
According to the Cancer Research Foundation of America, as many as 30 to 40 percent of the population over age 50 has pre-cancerous adenomatous polyps.
Colorectal cancer is cancer of the colon (the large bowel or large intestine) and/or the rectum. Most cases of colorectal cancer begin as non-cancerous polyps that grow on the wall of the colon or rectum. For reasons that are not fully understood, these polyps become cancerous.
Colorectal cancer affects men and women in equal numbers. While risk factors are important predictors, 75 percent of all new cases of colorectal cancer occur in individuals with no known risk factors other than age.
According to the National Cancer Institute, common signs and symptoms of colon cancer include:
- A change in bowel habits
- Diarrhea, Constipation (feeling that the bowel does not empty completely)
- Blood in the stool
- Stools that are narrower than usual
- General abdominal discomfort (frequent gas pains, bloating, fullness, and/or cramps)
- Weight loss with no known reason
- Constant tiredness
- Vomiting
If these problems persist, talk to your doctor and consult with a gastroenterologist.
The good news about colorectal cancer is that it is up to 90% curable if caught early enough. That is why screening is so important.
Colorectal cancer arises from benign growths in the colon known as polyps. The goal of screening is to detect and remove polyps before they have the opportunity to become cancerous. According to The Cancer Research Foundation of America as many as 30 to 40 percent of the population over 50 has pre-cancerous adenomatous polyps. Nearly all colorectal cancer develops from these growths in the colon and rectum.
Even if a cancer is detected during screening, it is often small and early in stage making curable surgery and treatment more likely.
Sadly, although physicians routinely recommend Pap smears, prostate cancer screenings, mammography and chest x-rays for patients, screening for colorectal cancer remains vastly underutilized. This may be the result of the uneasiness physicians and patients feel in discussing colorectal cancer. However, screening can save lives. Unfortunately, only 37 percent of colorectal cancer patients come to the doctor at an early stage when the cure rate is as high as 95 percent.
With 104,270 new cases of colorectal cancer and 52,980 deaths anticipated in the year 2021, there is no room for embarrassment or silence about colorectal cancer. The fact is, screening is safe, effective and readily available and a fecal occult blood test is the place to start.
- All men and women age 45 or older
- Men and women with a personal or family history of colorectal cancer or polyps, or a personal history of inflammatory bowel disease might need to be screened before age 45.
- Women who have a personal or family history of ovarian, endometrial or breast cancer may need to be screened for colorectal cancer before age 45. These people should talk to their doctors about when to begin screening.
The four major screening methods everyone should be aware of are:
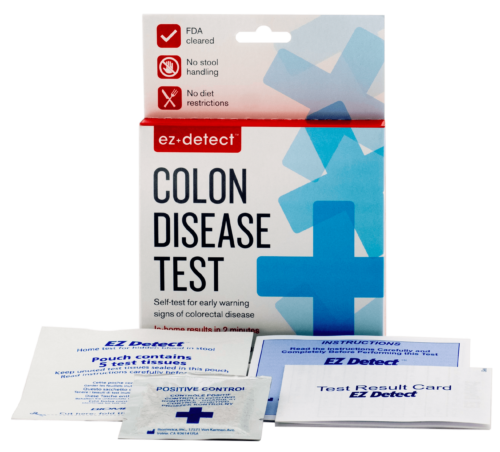
- Fecal Occult Blood Test (FOBT). This is a low cost screening test that checks for hidden blood in stool, one of the early warning signs of colorectal cancer. The most prevalent form of this test requires handling of stool, dietary restrictions, and laboratory processing: three major barriers to compliance. With EZ Detect™, these common barriers to compliance are eliminated. EZ Detect™ is the only non-invasive FDA cleared FOBT that can be performed and produce results at home that has no dietary restrictions and no handling of stool.
A positive FOBT result does not necessarily indicate colorectal cancer. There could be false positives or the test may also indicate ulcers, hemorrhoids, polyps, colitis, diverticulitis or fissures which may not show visible symptoms even though they are producing blood in the stool. EZ Detect™ can therefore serve as an early warning signal of other bowel troubles that need medical attention.
A negative FOBT does not necessarily indicate that colorectal cancer does not exist since not all polyps bleed or bleed all the time.
An FOBT cannot detect every colon problem or abnormality and does not replace an examination by a doctor or other diagnostic procedures. However, according to the University of Minnesota study, FOBTs are of great value in screening people for further examination and colonoscopy since FOBTs are such a low cost screening tool compared to colonoscopy. If there is a positive result with FOBT screening, the American College of Physicians recommends colonoscopy.
Recommended FOBT screening frequency: annually.
In the United States, where colonoscopy is generally safe and accessible, the preferred strategy for evaluating a positive result on a fecal occult blood test is colonoscopy.
- Colonoscopy - A colonoscopy is generally considered the gold standard of care in screening. In this procedure (typically performed by a gastroenterologist) a flexible tube with a light and camera on the end (called an endoscope) is inserted into the rectum and can visualize the entire colon. Biopsies can be taken and if identified, polyps can be removed at the same time. This exam does not usually cause pain, although it can be uncomfortable. (Most people say the preparation the day before the exam is the worst part.) Patients are generally given medication through a vein to make them feel relaxed and sleepy.
A colonoscopy usually is performed if someone is at high risk of colon cancer or after simpler tests (such as FOBT, sigmoidoscopy, DCBE or digital rectal exams) have found symptoms such as bleeding.
Recommended colonoscopy screening frequency: Every 8 to 10 years starting at age 45, or more frequently as recommended by physician.
- Sigmoidoscopy - A sigmoidoscopy is like a colonoscopy but only examines the lower third of the colon.
- Double-Contrast Barium Enema (DCBE) or Barium X-Ray - This is an x-ray examination of the rectum and entire colon performed in a hospital or clinic. The patient is given an enema containing white dye or barium, followed by an injection of air. The barium outlines the intestine and enables the doctor or health professional to take x-rays of the lower intestine.
The disadvantage of the double contrast barium enema, however, according to the American College of Physicians, is that an abnormal examination will require subsequent colonoscopy. "Moreover, and in greater importance in our view, a barium enema may not detect large (>1 cm) adenomas in about 40% of cases."
Fecal Occult Blood Test (FOBT). This is a low cost screening test that checks for hidden blood in stool, one of the early warning signs of colorectal cancer. The most prevalent form of this test requires handling of stool, dietary restrictions, and laboratory processing: three major barriers to compliance. With EZ Detect™, these common barriers to compliance are eliminated. EZ Detect™ is the only non-invasive FDA cleared FOBT that can be performed and produce results at home that has no dietary restrictions and no handling of stool.
Sigmoidoscopy is a visual examination of the rectum and lower portion of the colon, performed in a doctor’s office. This test can be uncomfortable, but it should not be painful. This screening method can detect 67 to 75 percent of polyps and 40 to 65 percent of colorectal cancers.
Double contrast barium enema (DCBE) or Barium X-Ray is an x-ray examination of the rectum and entire colon performed in a hospital or clinic. Your doctor or health professional will give you an enema containing white dye or barium, followed by an injection of air. The barium outlines the intestine and enables the doctor or health professional to take x-rays of the lower intestine.
Colonoscopy, the most thorough test procedure, is a visual examination of the rectum and entire colon, performed in a hospital or clinic. Using a slender, flexible lighted instrument called a colonoscope, a doctor (a gastroenterologist) looks at the inside walls of the full length of the colon. If abnormalities are found, they can be removed or a biopsy can be performed during the same procedure. This exam does not usually cause pain, although it can be uncomfortable. A general anesthesia is sometimes used for this procedure.
SOURCES: Centers for Disease Control and Prevention, American Cancer Society, National Cancer Institute
DISCLAIMER: The information provided here is not intended to replace the medical advice of your doctor or health care provider. Please consult your health care provider for advice about a specific medical condition. The information provided here is for educational purposes only. In no way should it be considered as offering medical advice. Biomerica, Inc. assumes no responsibility for how this material is used. Please check with a physician (such as a gastroenterologist) if you suspect you are ill.
Order EZ Detect™
Order EZ Detect™ today Risk Free! Your satisfaction is
unconditionally guaranteed or Biomerica will refund your
money in full. Any questions? Call 1-800-854-3002.



